It started out as an average April day, but as Dermot Tatlow drove home, he received a call that would lead to a global campaign to save his son’s life. When he heard the bad news, he knew immediately what his family was up against. “I pulled over and took a deep breath,” Tatlow says. “We thought we were out of the woods.” Tatlow’s 4-year-old son, Devan, had relapsed. After 17 months without needing any treatment, a routine biopsy showed Devan’s cancer had returned. “Our worst fears were realized,” says Tatlow.
Devan would need a marrow transplant. The prospect of going through chemotherapy for a second time and needing a transplant is daunting to anyone, but it’s especially harrowing if — like Devan — you’re of mixed race. Multiracial patients often have an incredibly hard time finding life-saving marrow matches. When Devan, whose father is Caucasian and mother is part Indian, was first diagnosed with leukemia, his family did a search of the international marrow registry that contains over 14 million donors and came up empty. “We knew there was nothing out there for him,” Tatlow says.
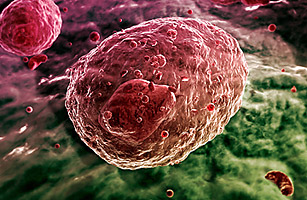
Compared to organ transplants, bone marrow donations need to be even more genetically similar to their recipients. Though there are exceptions, the vast majority of successful matches take place between donors and patients of the same ethnic background. Since all the immune system’s cells come from bone marrow, a transplant essentially introduces a new immune system to a person. Without genetic similarity between the donor and the patient, the new white blood cells will attack the host body. In an organ transplant, the body can reject the organ, but with marrow, the new immune system can reject the whole body.
To find a marrow match for anyone is hard. Even within one’s own family, the chances of finding one are only about 30%. According to the World Donor Marrow Association, while two out of three Caucasians find a match, the chances of a patient from another ethnic background can be as low as one in four. Despite rapid improvements in marrow registries around the world, the global registry is still disproportionately represented by the U.S., U.K. and Germany — all predominantly Caucasian countries. For a multiracial person, the chances are usually even worse. Athena Mari Asklipiadis, the founder of the California-based Mixed Marrow, one of the only outreach groups devoted to recruiting mixed race donors, says “the numbers are quite staggering … People compare it to winning the lottery.”
It’s difficult to ascertain the exact chances of finding a match for a mixed race person because the different combinations have different success rates, and the U.S.-based National Marrow Donor Program , which has about eight million donors in its registry, does not have statistics on the success rates of mixed race patients. But Asklipiadis maintains the rates are lower — much lower. “God forbid I need a match, because I’m a very rare combination,” Asklipiadis says of her mixed Japanese, Italian, Armenian, Egyptian and Greek background.
In the NMDP database, less than 3% of donors self-identify as mixed race. Though this approximately matches U.S. Census data, more mixed-race donors are needed given the sheer genetic diversity of the group. In both the U.S. and the U.K., people of mixed race are the fastest growing minority, and the population skews young. According to the 2000 U.S. Census, 41% of the mixed race population is under 18, meaning much of the mixed race population is too young to donate marrow, which requires donors to be at least 18. Asklipiadis says if more people of mixed race don’t step forward, “the numbers are just going to get worse.”
Part of the problem might be that there are a lot of negative misconceptions about donating marrow. Says Asklipiadis, “They assume it is more painful than it really is.” About 70-80% of the time, the donation is done through something akin to a five-hour blood donation. Blood is extracted from one arm into a machine that separates the needed cells, and then the remaining blood is returned through the other arm. Sometimes, a surgery is performed to extract liquid marrow from the back of the donor’s pelvic bone instead. This surgery, usually performed under local anesthetic, can leave one’s lower back a bit sore for a few days. Dr. Willis Navarro, the medical director for transplant services for the National Marrow Donor Program, compared it to being kicked by a horse, but he says being called on to save someone’s life is a wonderful opportunity. Says Navarro, “It’s an exciting feeling knowing you could be the only person in the world who can help that person.”
Registering is easy, says Victoria Moffett, a spokesperson at the Anthony Nolan Trust, a U.K.-based marrow registry. The process varies a little from country to country, but in most places if you’re between 18 and 60, a registry will send you a free kit in the mail with a questionnaire. You’ll then either spit in a tube or swab your cheeks, send it to a lab, and won’t be contacted unless there’s a match. “It’s very easy to do, and you could save someone’s life,” Moffett says.
Knowing that there weren’t enough mixed race donors, Devan’s parents did everything they could to raise awareness and get people — especially of mixed race — to sign up for a marrow registry. Using Facebook and Twitter, word of Devan’s plight spread around the world. Kim Kardashian, Paris Hilton, Nicole Ritchie, Buzz Aldrin and Aston Kutcher, to name only a few, tweeted about Devan. Over 20 million people viewed calls on Twitter for people to join a registry. “I can’t be cynical about Paris, Kim and Nicole Ritchie anymore,” Tatlow says. “Part of the reason the campaign did so well is that people think, ‘My God is that all it takes?'”
Tatlow recently received another call, this one bearing good news. Devan’s doctor informed the family a cord blood match had turned up. It’s not a perfect solution, but Devan’s doctor says it’s good enough. Blood from the umbilical cord is rich in blood-forming cells, and cord blood doesn’t have to match quite as closely as marrow from an adult. In the U.S. registry, compared to the over eight million potential marrow donors, there are only about 160,000 cord blood units. Tatlow urged pregnant women to donate their cord blood: “For pregnant women, your baby’s umbilical cord, which is otherwise thrown away, can save a life. It just seems like a very simple thing to do for the greater good of mankind.”
Devan’s ordeal isn’t over. He still needs to go through weeks of chemotherapy and then a dangerous transplant and recovery period. “It’s pretty tough as a parent to see our own child facing this road ahead,” Tatlow says. “But this is a lifeline for us.” Asklipiadis says that getting people to realize that a simple act of donating cord blood or getting on a marrow registry can save a life is the most important step. If a person needs marrow transplant, “it’s not a death sentence,” she says. “We can save each other.”
See TIME’s Pictures of the Week.
See the Cartoons of the Week.